Cupid is in the air! What a wonderful time to reflect on our love relationships. Obviously, we should be appreciative, kind, loving, understanding, and helpful year-round, but Valentine’s  Day brings an extra little reminder to pay special attention to those we love. So why, you might wonder, is a specialist in regenerative and longevity medicine talking about love? The answer is surprisingly simple: the love in your life, or lack thereof, has a profound effect on your health and how long you live. Day brings an extra little reminder to pay special attention to those we love. So why, you might wonder, is a specialist in regenerative and longevity medicine talking about love? The answer is surprisingly simple: the love in your life, or lack thereof, has a profound effect on your health and how long you live.
I’m not just referring to the fact that having unprotected intimacy at least twice per week has been shown to reduce your risk of having a heart attack (yes, this has actually been studied!) or dying of any cause. Nor am I solely referring to the fact that happily married people live longer, on average, than unmarried people. You don’t have to be in a committed intimate relationship to enjoy the health benefits of love. Your love for a parent, child, sibling, friend, or even a pet can provide not only companionship and comfort, but also a happier and longer life.
It turns out that relationships are a more powerful predictor of longevity than exercise, diet, blood pressure, cholesterol, weight, smoking, and any other factor studied. The science is clear: Loving relationships trigger beneficial hormones, reduce stress, boost immune function, and even affect how our cells age.
 Unlike tigers and bears, the human body was not designed for solitary living. We are social creatures by design. Lack of regular social contact is a major risk factor not only for a shorter life, but also for disease. Sadly, 1 in 2 adults in America suffers from loneliness, which is as deadly as smoking 15 cigarettes a day. This is why, at Prestige Wellness Institute, we stress the importance of creating and maintaining nurturing relationships throughout your lifespan. It is also why we urge our patients—regardless of their age or marital status—to involve themselves in churches, clubs, and/or civic or charitable organizations. Humans have an innate need to feel needed and useful. We need to make a difference in the world, even if it’s only a difference in one person’s world. We need to feel cared about. And we need other people with whom to share our genuine love. Unlike tigers and bears, the human body was not designed for solitary living. We are social creatures by design. Lack of regular social contact is a major risk factor not only for a shorter life, but also for disease. Sadly, 1 in 2 adults in America suffers from loneliness, which is as deadly as smoking 15 cigarettes a day. This is why, at Prestige Wellness Institute, we stress the importance of creating and maintaining nurturing relationships throughout your lifespan. It is also why we urge our patients—regardless of their age or marital status—to involve themselves in churches, clubs, and/or civic or charitable organizations. Humans have an innate need to feel needed and useful. We need to make a difference in the world, even if it’s only a difference in one person’s world. We need to feel cared about. And we need other people with whom to share our genuine love.
But what happens when relationships are less than ideal? Far too many of us grew up in homes, communities, and churches where “love” wasn’t really love. Approval was conditional. Behavior was unpredictable. Affection was weaponized or even completely absent. Genuine concern for the wellbeing of another was replaced with control. Rules established to prevent harm and foster healthy growth were replaced with manipulation to satisfy the selfish desires of the rule-giver.
Children who grow up in these conditions often unknowingly perpetuate them in their own relationships with intimate partners, children, friends, and coworkers. Put another way, childhood programming plays out in adult relationships. In addition to causing mental illness, unhealthy relationships significantly increase risk of chronic disease and shortened life. 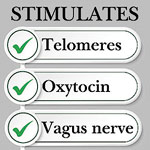 These findings have been confirmed by research on Adverse Childhood Events (ACEs). The ACEs questionnaire asks ten questions about one’s childhood. For example, one ACE is identified by the following question: “Did a parent or other adult in the household often swear at you, insult you, put you down, or humiliate you, or act in a way that made you afraid you might be physically hurt?” Adults who had at least four ACEs have a 12x greater likelihood of developing alcoholism, drug abuse, depression, and suicide attempts. And adults who endure abusive relationships at any time in their lives have a much greater risk of heart disease, diabetes, and early death. These findings have been confirmed by research on Adverse Childhood Events (ACEs). The ACEs questionnaire asks ten questions about one’s childhood. For example, one ACE is identified by the following question: “Did a parent or other adult in the household often swear at you, insult you, put you down, or humiliate you, or act in a way that made you afraid you might be physically hurt?” Adults who had at least four ACEs have a 12x greater likelihood of developing alcoholism, drug abuse, depression, and suicide attempts. And adults who endure abusive relationships at any time in their lives have a much greater risk of heart disease, diabetes, and early death.
What can we do when relationships aren’t all they were cracked up to be? Of course, professional therapy can be invaluable. The website www.psychologytoday.com provides access to both local and national therapists, in-person and virtual. But you can do a lot on your own as well. A good start is to educate yourself about what love is and what it is not. With this knowledge, you can better understand how to truly love those around you, how to help them love you in return, and how to recognize behaviors in others that warrant intervention. If education is not enough, setting new boundaries may be required, focusing on acceptable vs. unacceptable behaviors instead of blanket generalizations. For example, “When you promise to mow the lawn on Friday, I need to know it is going to happen, without excuses” is much more constructive than saying “You need to stop being such a narcissist.”
| LOVE |
NOT LOVE |
| Steady affection, emotional regulation, reliability, care |
Constant contact, emotional highs and lows, obsession mistaken for passion |
| Encourages friendships, individuality, independence |
Isolation from friends and family, relationship becomes your whole world |
| Trust, freedom to grow, emotional security |
Possessiveness disguised as devotion; suspicion; anxiety when apart |
| Honors boundaries, respects differences, collaborative decision-making |
Monitoring, manipulation, dictating choices |
| Calm, grounded, dependable, safe disagreement |
Drama, punishment, emotional whiplash, unpredictable |
In some cases, violation of boundaries may require ending a friendship, distancing oneself—at least temporarily—from a family member, or terminating an intimate relationship. Supportive family members, friends, professional counselors, and sometimes even law enforcement can be enormously helpful in circumstances like this, as people who cannot recognize the difference between love and enslavement can become volatile and even dangerous.
It is also essential that we teach our youth to recognize these “loving” and “non-loving” behaviors. With self-worth being under constant bombardment from so many directions these days, youth need all the help they can get in learning to choose nurturing friendships. Rather than simply telling them who good friends are, we can teach them how to recognize and choose them. When it comes to dating, an understanding of how true love behaves will help youth identify relationships that lead to health, happiness, and longevity vs. those that will not.
If you are in an intimate relationship, you may recall that love was effortless in the beginning, and you were certain you were meant for each other. Once life “happened”, you learned that true love requires work. Friendship requires work, too. In both cases, we can use Valentine’s Day as a good reminder to cherish our loved ones, uplift them as often as possible, practice kindness, forgive, and hug often. We’re never going to overdose on oxytocin. Let’s lengthen those telomeres!
If you are looking for additional tools to enable you to prolong your lifespan and your healthspan, call Prestige Wellness Institute at (435) 210-0184 in Northern Utah and (435) 259-4466 in Southeastern Utah.
.
|

Health insurance can feel confusing. Between unfamiliar terms, unexpected bills, and different rules for different plans, it’s not always clear what to expect. If you live in or around Moab, this guide explains the basics of how insurance and billing work at Moab Regional Hospital, how to avoid surprises, and where to turn if costs become a concern.
THE FIRST STEP: BRING YOUR INSURANCE CARD
The first step to correct billing—whether you visit Moab Regional Hospital, the Emergency Room, Urgent Care, Specialty Clinics, or Family Medicine—is to bring your current insurance card.
Your insurance card allows our registration team to:
• Confirm your coverage
• Submit charges correctly to your insurance
• Reduce delays or billing errors
Even if you’ve been to Moab Regional Hospital before, insurance information must be re-entered each year.
WHY YOU MIGHT RECEIVE MORE THAN ONE BILL
Many patients are surprised to receive more than one bill after a hospital visit. This is common and doesn’t necessarily mean anything was billed incorrectly.
For example:
• Emergency Room bills come from CarePoint
• A lab may bill separately for blood work
• Our radiology partner, Utah Imaging Associates, bills for a CT scan
These services may come from different hospital partners, even though they all happened during the same visit. Each bill should match an Explanation of Benefits (EOB) from your insurance, which shows what was billed, what insurance paid, and what you may owe.
If something doesn’t look right, Moab Regional Hospital’s billing team can help review it with you.
PREAUTHORIZATION: WHAT IT IS & WHY IT MATTERS
Some tests, scans, or procedures require preauthorization, which means your insurance company must approve the service before it happens.
• Preauthorization rules depend on your specific insurance plan
• Some plans require approval for MRIs, CT scans, or certain procedures
• Others do not
Your provider’s office will often help request authorization, but approval is ultimately determined by your insurance. If authorization is denied, insurance may not pay for the service, so it’s important to check ahead when you can.
When scheduling planned care, it’s always okay to ask:
• “Does this require preauthorization?”
• “Has my insurance approved this?”
IF YOU DON’T HAVE INSURANCE: GOOD FAITH ESTIMATES
If you are uninsured or choosing not to use insurance, you have the right to request a Good Faith Estimate.
A Good Faith Estimate is:
• An expected cost of your care before you receive it
• Based on the known services planned at that time
• Designed to help you understand and plan for costs
Actual charges may change if additional care is needed, but the estimate provides transparency and helps reduce surprises.
TALKING WITH YOUR DOCTOR & CHARGES
Different parts of your visit may be billed separately. For example:
• A routine office visit
• A longer or more complex discussion
• A procedure performed during the visit
• Additional tests ordered
These charges are based on the type and complexity of care provided, not just the length of time spent. Your provider’s documentation helps determine how services are billed.
UNDERSTANDING COPAYS & DEDUCTIBLES
Copay
A copay is a set amount you pay at the time of your visit (for example, $30 for a clinic visit).
Deductible
Your deductible is the amount you must pay each year before your insurance starts covering certain services.
For example:
• If your deductible is $2,000 and you haven’t met it yet
• You may be responsible for more of the bill early in the year
• Once the deductible is met, insurance usually pays more
Every plan is different, and Moab Regional Hospital’s billing team can help explain what applies to your visit.
MEDICARE & MEDICAID CAN HELP
Medicare may help:
• Adults age 65 and older
• People with certain disabilities
• Individuals with specific medical conditions
Medicaid may help:
• Low-income adults and families
• Pregnant individuals
• Children
• Some people with disabilities
Many people qualify and don’t realize it. These programs can significantly reduce medical costs. MOab Regional Hospital’s financial assistance staff can help determine if you may be eligible and guide you through the next steps.
HOW MOAB REGIONAL HOSPITAL HELPS
Moab Regional Hospital is constantly working to improve billing clarity and support patients through the financial side of care. Our goal is to help people receive the care they need—without confusion or unnecessary stress.
“We encourage patients to reach out to us at any time. Our billing team and financial assistance navigator are here to help explain bills, explore available assistance options, and answer any questions you may have. We are committed to helping people get the care they need and supporting them through the process of paying for that care.” — Camia McGuire, Business Office Manager.
Need Help or Have Questions?
FINANCIAL ASSISTANCE & BILLING QUESTIONS: 435-719-3536
Calling early can help prevent confusion and give you more options. Moab Regional Hospital’s team is here to help you understand your bill and find solutions that work for you and your family.
Moab Regional Hospital Financial Support in 2025
Financial Assistance
• Patients helped: 456
• Total assistance provided: $1,431,156
Uninsured Discounts
• Patients helped: 2,977
• Total discounts provided: $2,919,890
Moab Regional Hospital is committed to supporting patients who need care but face financial barriers. These programs help ensure access to essential healthcare services for individuals and families in our community.
|